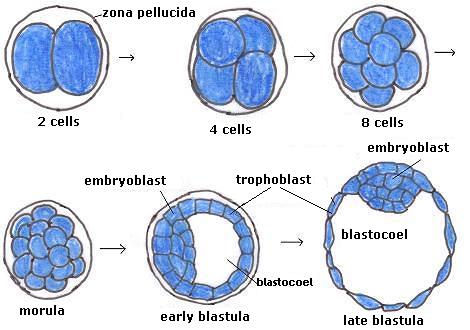
You might recall that last time we had 12 eggs retrieved, 9 off which were immature, 3 of which were mature and fertilized. By day 5, we had 1. It went for testing and came back aneuploid: 49 chromosomes.
This time we had 29 eggs retrieved, 21 of which were mature, 16 of which fertilized, 12 which survived to day 5, and are now off to testing.
At this point last time we had one, this time we have 12. So what’s the deal?
A few things:
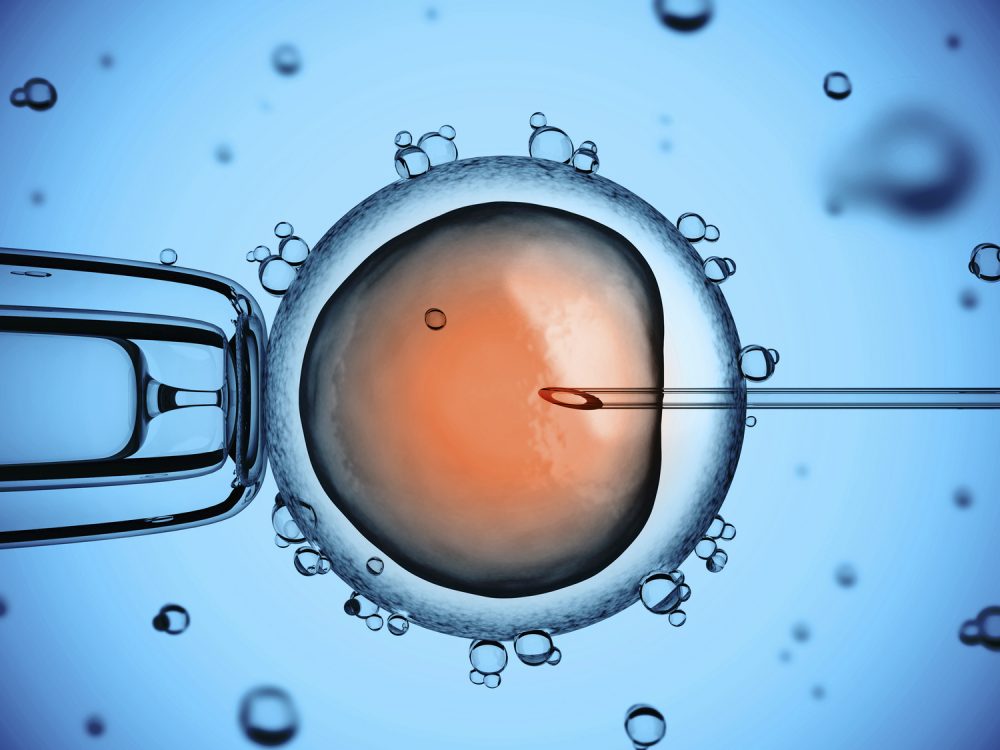
1. Different drugs, and different doses of drugs. Last time I took 225 IUs of Follistim (which contains Follicle Stimulating Hormone, or FSH) in both the morning and evening. This time I took 300 IUs in the evening only (about 40% more) and a different drug that does the same thing, called Menopur, in the morning. Menopur contains FSH, but it also contains Leutenizing Hormone (LH), where as Follistim does not. Don’t quote me on this, but I believe the doctor said that Menopur is derived from the urine of menopausal women.
Also this time I took a drug called Omnitrope, instead of Low Dose HCG (Human Chorionic Gonadotropin). Omnitrope is a somatropin, and helps cells grow. Don’t ask me the difference betweeen a gonadotropin and a somatropin.
Each of these drugs (FSHs, LH, tropins) push the development of eggs.
Meanwhile, you want to prevent premature ovulation, so while we are pushing the eggs to grow, we are also pushing back with Ganirelix to ensure they don’t ovulate. Last time if I even took Ganirelix (I don’t think I did?) I took it once. This time I took it for 4 days before the retrieval.
In general I got the sense that the doctor was pushing growth harder, and pushing harder on premature ovulation. Hence, the higher numbers.
[Side note: part of the reason we went to Oregon Reproductive Medicine for round 2 is that the doctor there looked at my round 1 results and suggested these changes. Meanwhile, the doctor from round 1 suggested no changes. See lead-off quote.]
2. Additional supplements. In addition to lots of eggs, the other thing you want is high quality eggs. Dexamethazone was prescribed because it can help with that. Same with CoQ10, DHA/Omega-3’s, a baby aspirin (for more blood flow to the scene). I felt like my own private pharmacy some days, with all these pills. It appears that this helped, because of my 12 eggs, graded on 2 characteristics, 10 were graded AA, and two were graded BB. So they were high quality indeed.
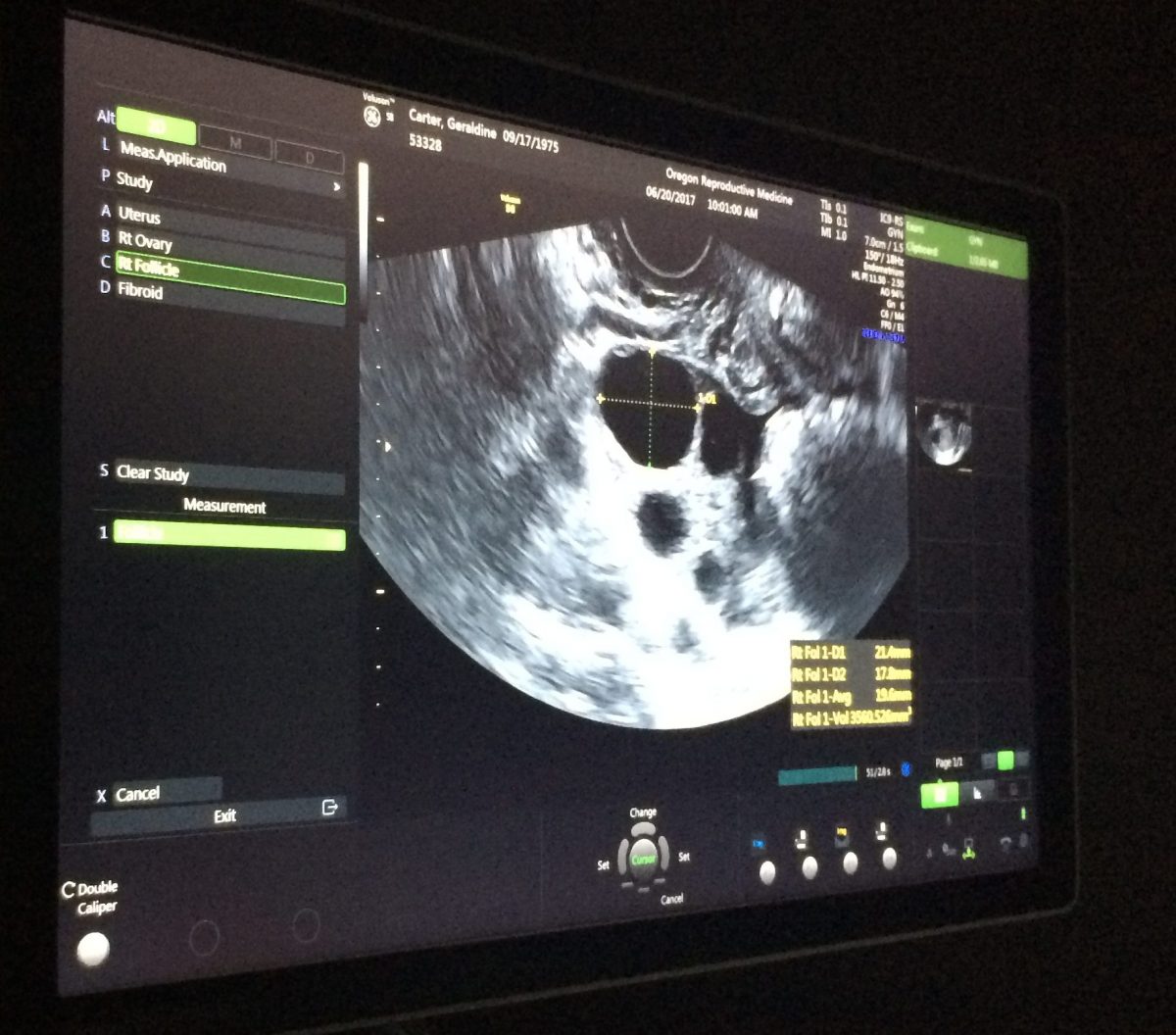
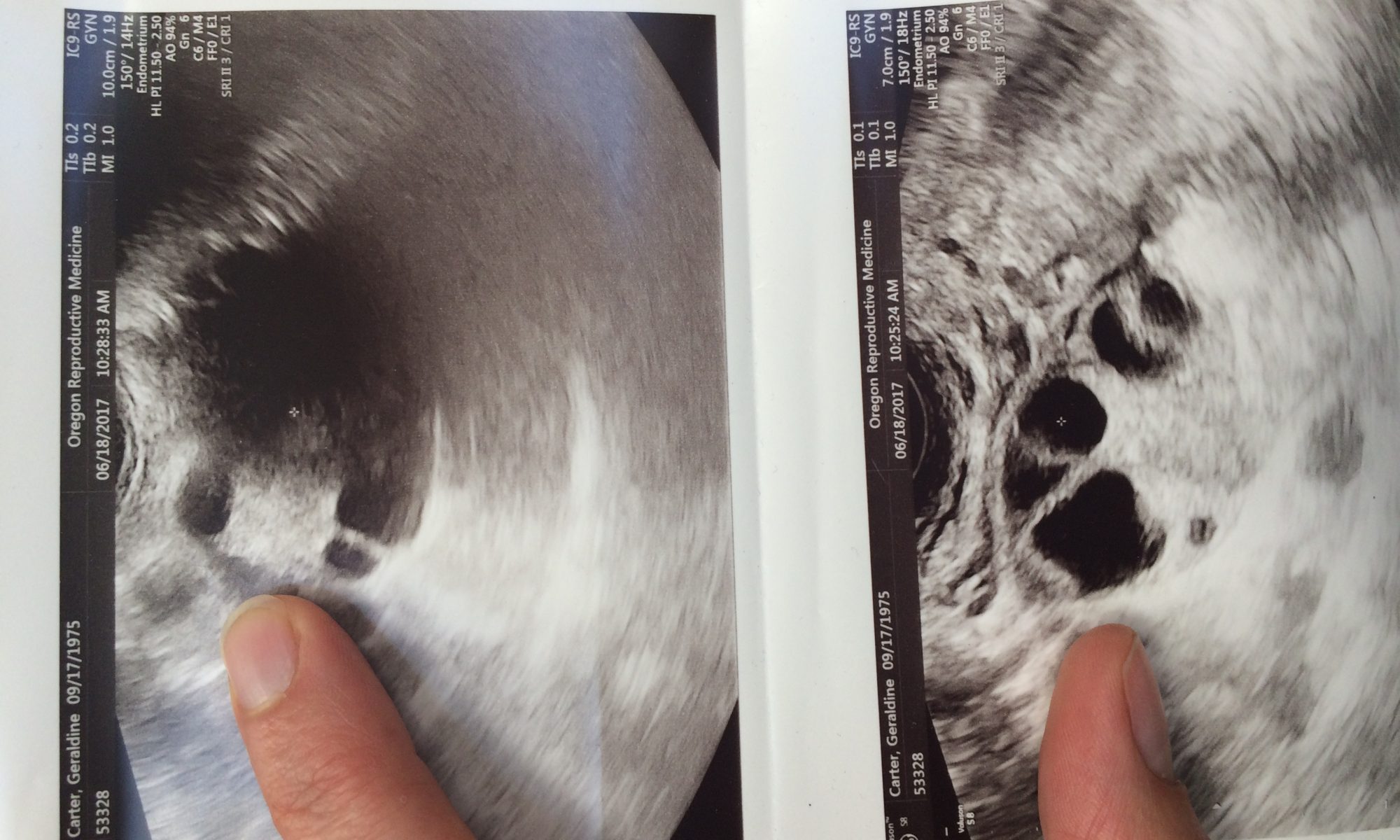
3. Data from the previous round. The value of these data is not to be underestimated. At my day 10 ultrasound, when they would normally say, looks great, we will retrieve on day 12, what happened instead was my doctor was comparing the data from my Round 1 eggs – comparing sizes, and outcomes. What he saw was that last time my eggs were around 15mm on day 10, and 75% were immature. This time around, we were in the same place – eggs around 15mm. He made the call to hold off on the retrieval one more day – so my retrieval was day 13, rather than the more common day 12, in order to give the eggs one more day to mature. Clearly it was the right call.
4. Meditation. I started nearly every day with a 10 minute visit to my ovaries. No joke. I brought each follicle into view in my mind’s eye, greeted it with loving kindness, thanked it for being here, and encouraged it to have the right chromosome count. I looked around and asked if there were more follicles that wanted to join the brigade, and let them know that it was safe to be part of this party and that they were most welcome to come along.
There you have it – four factors that made the difference.